A plain-English guide for U.S. readers 50+: what your pancreas does, simple daily habits that help, and when to call your clinician.
The pancreas—the small gland that releases digestive enzymes (to break down fat, protein, and carbs) and hormones like insulin (to steady blood sugar)—can use a little extra care at this stage. If you’ve noticed heavier meals sitting longer, afternoon energy dips, or more bloating than before, small daily shifts can make digestion feel easier and keep your energy steadier.
Below we’ll share pancreas-smart habits that fit a normal U.S. kitchen and routine: when and how to eat, simple food swaps that are easier to digest, hydration cues that actually stick, movement that nudges enzymes along, and signs it’s time to check in with your clinician. If you manage diabetes, take pancreatic enzymes, or have a history of pancreatitis, bring these ideas to your care team so they can tailor them to you.
Table of Contents
- Why your pancreas matters after 60
- Gentle, senior-friendly habits (low effort, real payoff)
- Pantry quick list: easy wins
- When to call your clinician
- Useful, trustworthy resources
- Q&A
- Bottom line
Why your pancreas matters after 60
This small organ does two big jobs:
- Digestion: it releases enzymes that break down fat, protein, and carbs so meals don’t “sit heavy.”
- Blood sugar control: it makes insulin and glucagon to keep glucose in a healthy range.
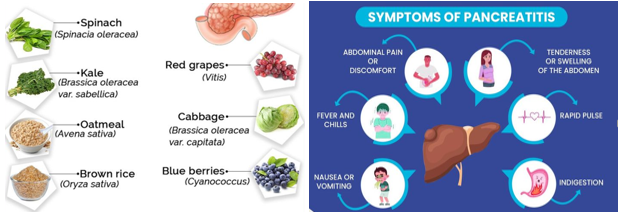
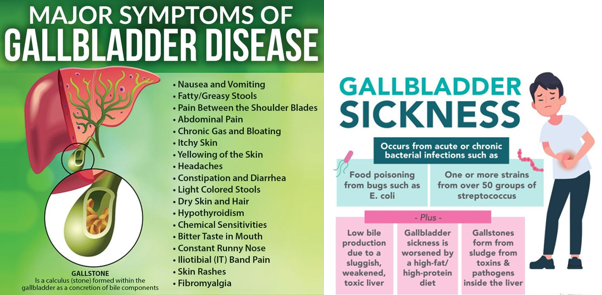
If things go off track, you might notice gas, floating/greasy stools, belly pain after meals, sudden fatigue, or unexplained weight changes. Ongoing symptoms deserve a check-in with your doctor—conditions like pancreatitis or exocrine pancreatic insufficiency (EPI) need proper testing and treatment.
Gentle, senior-friendly habits (low effort, real payoff)
1) Build steady, fiber-forward plates
Use a simple formula at each meal: fiber + lean protein + healthy fat. Think oatmeal with berries and nuts; beans with greens and olive oil; yogurt with chia. Increase fiber gradually and drink water to limit gas.
Related reading: What Foods Cause Inflammation? (smart swaps you can actually keep)
2) Move most days (short sessions count)
Aim for walking, light cycling, or water aerobics on most days, plus 2x/week gentle strength and some balance work. Movement helps insulin do its job, which supports both energy and appetite control.

3) Be “enzyme-aware”
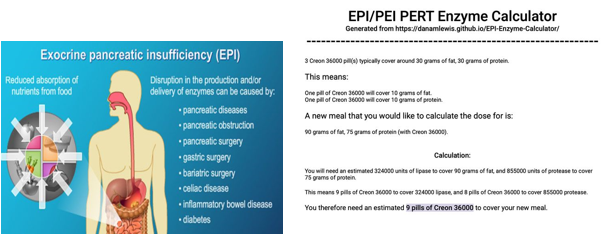
Persistent bloating, pale/oily stools that float, or weight loss can point to EPI. Doctors can prescribe pancreatic enzyme replacement therapy (PERT) when needed. Don’t guess—get evaluated, then tailor meals with your clinician or dietitian.
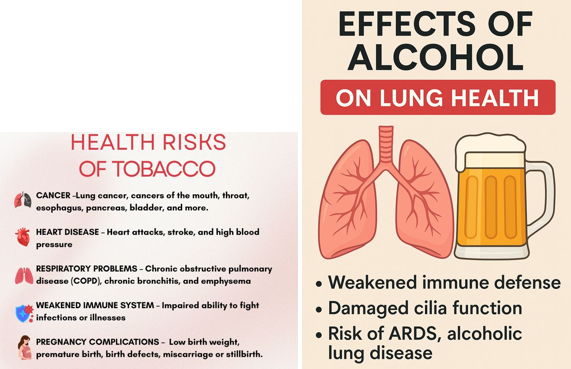
4) Keep alcohol modest; skip tobacco
Heavy drinking and gallstones are common pancreatitis triggers. If you drink, keep it light and consistent; if you smoke, ask about proven quit aids—your pancreas (and heart) will thank you.
5) Watch gallbladder signals
Sharp upper-abdominal pain (often to the back), fever, vomiting, or yellowing of the eyes/skin can mean a blocked duct. That’s urgent—seek care.
6) Sleep, stress, and weight in a reasonable lane
Regular sleep and a calm daily rhythm help insulin sensitivity. Pair that with short, daily walks and produce-heavy meals for steadier energy.

Also helpful: Best Gentle Constipation Relief for Seniors (fiber and hydration tips that also ease digestion)
Pantry quick list: easy wins
- Fiber staples: oats, barley, rye crackers, beans/lentils, chia, raspberries, broccoli, leafy greens. Add slowly.
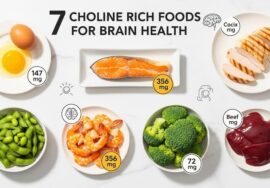
- Protein with a light touch: eggs, yogurt, tofu, fish, chicken; spread protein across meals to avoid sugar dips.
- Better fats: olive or canola oil, avocado, nuts/seeds; trim heavy saturated fats to support metabolism.
Prefer a calm, lower-caffeine routine? Try Matcha Benefits for Older Adults for a gentle comparison of morning drinks.
When to call your clinician
Don’t wait if you have severe or worsening upper-abdominal pain, pain that reaches the back, fever, vomiting, a fast heartbeat, shortness of breath, or jaundice. Also call for ongoing greasy/floating stools, stubborn diarrhea/constipation, or unplanned weight loss.
Useful, trustworthy resources
- NIDDK: Pancreatitis—Symptoms, Causes, Treatment
- Cleveland Clinic: Exocrine Pancreatic Insufficiency (EPI)
- CDC: Physical Activity for Older Adults
- American Diabetes Association: Exercise & Blood Sugar
- American Heart Association: Healthy Fats 101
More from KeepFitQuote: Best Foods for Body Detox
Q&A
- What does the pancreas do?
Breaks down food with enzymes and helps control blood sugar with hormones. - What’s the simplest habit that helps?
Build fiber-forward plates and move a little every day. - How much activity should I aim for?
About 150 minutes/week of moderate activity plus strength and balance work. - Which foods are easiest on digestion?
Oats, beans, berries, yogurt, tofu/fish/chicken, olive oil, nuts, and plenty of vegetables. - Are healthy fats okay?
Yes—favor unsaturated fats (olive/canola, nuts, avocado) over heavy saturated fats. - What are red-flag symptoms?
Severe upper-abdominal pain (especially to the back), fever, vomiting, yellow eyes/skin—seek care now. - What is EPI?
Exocrine pancreatic insufficiency—not enough enzymes; may cause greasy stools, gas, and weight loss. It’s treatable. - Do I need enzyme pills?
Only if your clinician diagnoses EPI or a related condition; self-prescribing can miss the real cause. - Does alcohol matter?
Yes. Heavy use raises pancreatitis risk. Keep intake modest or skip. - What about smoking?
Smoking increases pancreatic cancer risk; quitting helps across the board. - How do fiber and water work together?
Add fiber gradually and drink water so stool stays soft and comfortable. - Any quick plate formula to remember?
Half vegetables/fruit, a palm of protein, a thumb of healthy fat, and a fist of whole grains—adjust for appetite and meds.
Bottom line
Keep it simple and repeatable: walk most days, build fiber-rich plates, use healthy fats, keep alcohol modest, and don’t smoke. If new belly pain or greasy stools show up, call your clinician—early care protects digestion and energy..