Not all forgetfulness means dementia. But a pattern of short-term memory slips, word-finding trouble, getting lost on familiar routes, mistakes with bills, new mood or behavior changes, sleep disruption, or safety issues may signal early Alzheimer’s or another dementia and deserves a medical evaluation.
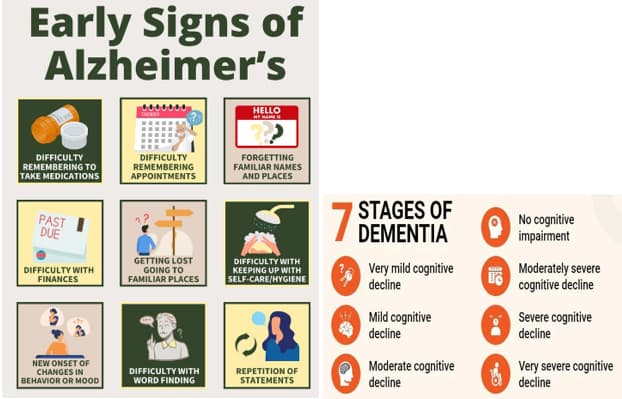
Table of Contents
- Normal Aging vs. Early Dementia
- At-Home Early Signs Checklist
- Mild Cognitive Impairment (MCI)
- When to See a Doctor (U.S.)
- Early-Action Brain-Health Steps
- FAQs
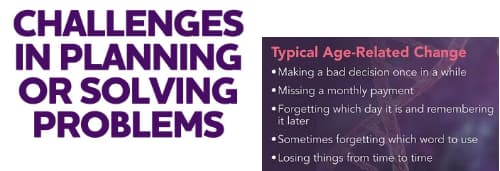
Normal Aging vs. Early Dementia
Normal aging can include: occasionally misplacing items, momentarily blanking on a name, or needing more time to learn new tech.

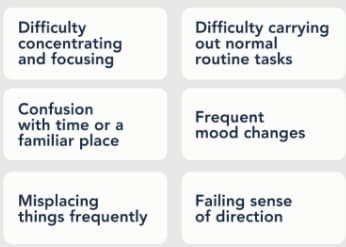
Possible early dementia/Alzheimer’s often shows progressive changes that begin to disrupt daily life:
- Repeating questions or stories; missing important dates and appointments
- Word-finding trouble and losing the conversational “thread”
- Getting disoriented on familiar routes; time/place confusion
- Decline in planning and organization (recipes, multi-step tasks)
- Money mistakes, unpaid bills, increased vulnerability to scams
- New mood, personality, or behavior changes (apathy, anxiety, irritability)
- Safety issues (stove on, doors open, risky purchases)
Helpful overviews:
At-Home Early Signs Checklist
Use this educational checklist to track patterns over 4–6 weeks. If several items apply—and others notice—book a medical visit. (Not a diagnostic tool.)
- Short-term memory slips that disrupt routines (e.g., repeating questions, forgetting recent conversations or events)

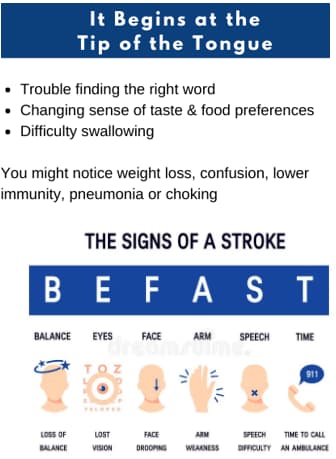
- Word-finding trouble or stalled conversations; losing the “thread”
- Navigation issues (getting turned around on familiar routes)
- Planning & bills: missed payments, math errors, trouble following steps/recipes
- Misplacing essentials and being unable to retrace steps

- Judgment changes (risky purchases, scams, poor safety choices)
- Social withdrawal or loss of interest in hobbies

- Mood/personality changes (apathy, anxiety, irritability)
- Sleep disruption or day/night confusion that’s new

- Vision/space challenges (depth perception, recognizing objects)

Tip: Keep a simple log (date, example, who noticed). Bring it to your appointment.
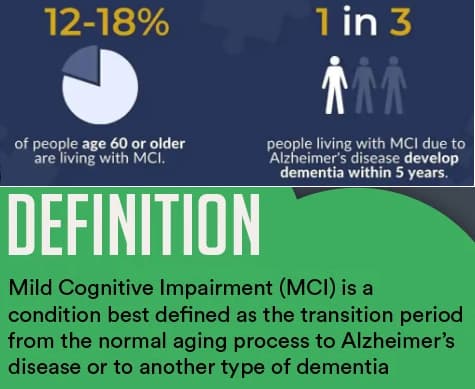
Mild Cognitive Impairment (MCI)
MCI is an “in-between” stage: noticeable change (especially memory or language) but most daily function remains. MCI increases the risk of later dementia, including Alzheimer’s. Early evaluation matters.
- Learn more: Mayo Clinic: Mild Cognitive Impairment
When to See a Doctor (U.S.)
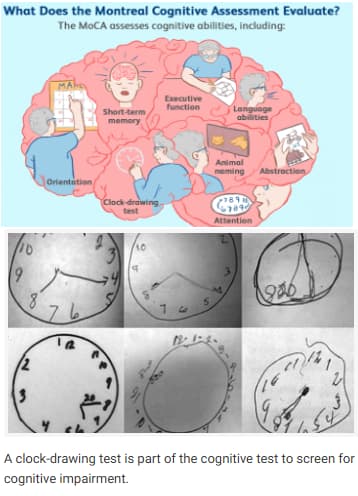
- If multiple checklist items persist for months, ask for a cognitive evaluation. Expect history, short memory/thinking tests, lab work (e.g., thyroid, B-12), and sometimes imaging or specialized biomarker tests.
- For adults 65+ without symptoms, the USPSTF says evidence is insufficient for routine dementia screening. This does not apply when you or family notice signs—then an evaluation is appropriate.
Useful U.S. resources:
Early-Action Brain-Health Steps
These do not diagnose or cure, but they support brain health while you seek care:
- Track patterns in a notebook or phone note (4–6 weeks)
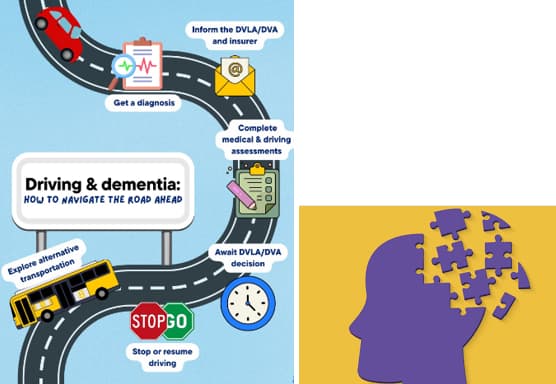
- Safety first: driving review, stove/oven routines, medication and finance safeguards
- Lifestyle supports: regular physical activity, social connection, hearing care, sleep routines, and heart-healthy habits (see CDC risk-reduction guidance)
- Care team: primary care clinician, eye/hearing checks; ask about MCI assessment if patterns persist
Suggested (internal) further reading on KeepFitQuote:
FAQs
1) What early memory issues are not “just aging”?
Frequently repeating questions, missing important dates, or heavy reliance on reminders for routine tasks.
2) Is word-finding trouble a red flag?
Occasional tip-of-the-tongue moments are common; persistent difficulty holding everyday conversations may be an early sign.
3) Can getting lost locally be an early clue?
Yes—time/place confusion or turning around on familiar routes can appear early.
4) What is Mild Cognitive Impairment (MCI)?
An intermediate state with measurable cognitive change but relatively intact daily function; it raises dementia risk.
5) When should I talk to a doctor?
If several checklist items persist for months and others notice changes, seek evaluation.
6) Do mood or personality shifts matter?
Yes—apathy, anxiety, irritability, or withdrawal can appear early.
7) What medical tests are common?
History, brief cognition tests, labs (e.g., thyroid, B-12), plus imaging or biomarkers when appropriate.
8) Are vision or spatial issues part of early signs?
They can be—depth perception or object recognition changes may occur.
9) Do bill-paying mistakes count?
Yes—new, repeated errors or missed payments are concerning.
10) Does everyone with MCI develop dementia?
No. Some remain stable or even improve, but MCI increases risk, so monitoring is important.
11) Is routine screening recommended for symptom-free adults 65+?
The USPSTF finds insufficient evidence for routine screening in those without symptoms.
12) What should families track?
Dates, concrete examples, safety concerns, and who noticed the change.