Table of Contents
- Introduction
- What Changes After 60 (and why “little habits” matter)
- Talk With Your Doctor: Screening & Decisions in Your 60s
- Everyday Food Habits That Are Kind to Your Prostate
- Budget Pantry List (cheap, simple, U.S. grocery staples)
- Hydration & Bladder-Friendly Timing (day vs. evening)
- Move More: Walking, Strength, and Pelvic Floor Basics
- Supplements: What’s promising—and what probably isn’t
- Ben Stiller’s PSA Story (Hollywood reminder to get informed)
- A One-Week “Natural Prostate Routine” Starter Plan
- FAQs
1) Introduction
Hitting your 60s doesn’t mean surrendering comfort, sleep, or bathroom freedom. Most men do best with a simple, repeatable routine: smarter meals, better fluid timing, light daily movement, and an informed chat with a clinician about screening. The goal here isn’t perfection—it’s consistency.
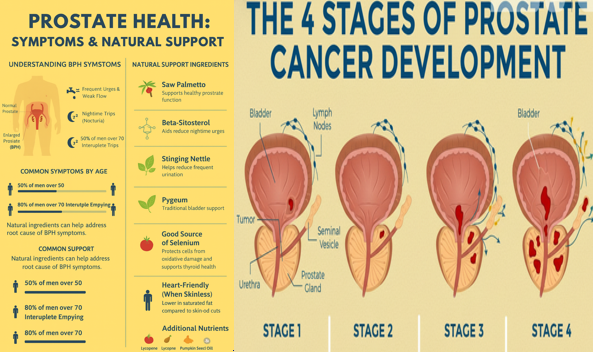
2) What Changes After 60 (and why “little habits” matter)
Age can make the lower urinary tract more sensitive to caffeine, alcohol, evening fluids, and spicy foods. The upside? Gentle tweaks—more vegetables and whole grains, steady activity, weight control, and good sleep—support vascular and urinary health at once. Practical measures like avoiding large drinks late at night, limiting bladder irritants, and staying active are standard first-line advice in urology. American University Alumni Network+1
3) Talk With Your Doctor: Screening & Decisions in Your 60s
For men 55–69, PSA screening is a personal decision after a risks-and-benefits conversation with your clinician; routine screening is not advised ≥70. Knowing your family history and preferences matters here. If you choose to screen, do it with eyes open about false positives and over-treatment. USPSTF+2USPSTF+2

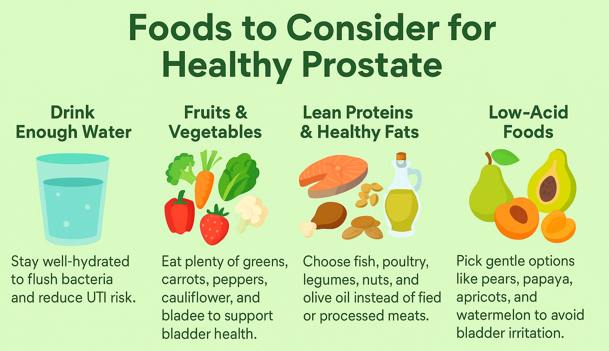
4) Everyday Food Habits That Are Kind to Your Prostate
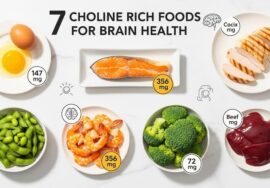
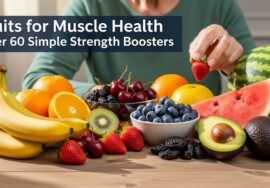
- Vegetable-forward plates. More greens, beans, berries, and olive oil (a Mediterranean-style pattern) help vascular health and weight control—both tied to urinary symptoms. Mayo Clinic
- Tomatoes & lycopene (food first). Evidence favors whole-food lycopene (tomatoes/tomato paste) over supplements for long-term protection; think tomato soup or sauce a few times a week. PMC+1
- Tea time, not pill time. Green tea catechins show preventive promise in select groups, but treat them as a supportive habit, not a cure. PMC+1
- Easy wins: swap soda for water, load half your plate with produce, and make beans your budget protein twice a week. Mayo Clinic
👉 Keep readers on-site: What Herbs Are Good for Healing.
5) Budget Pantry List (cheap, simple, U.S. grocery staples)
- Canned tomatoes/tomato paste (for lycopene-rich sauces) PMC
- Frozen mixed vegetables, spinach, broccoli
- Oats, brown rice, whole-wheat pasta
- Beans/lentils (canned or dry)
- Olive oil, walnuts (smart fats)
- Green tea bags
- Low-sodium broths and spices to cut salt cravings Mayo Clinic
6) Hydration & Bladder-Friendly Timing (day vs. evening)
Hydrate earlier in the day. Cut back on large fluids 2–3 hours before bed to reduce nighttime bathroom trips. If you love coffee or a beer, try earlier-day servings, smaller cups, or decaf. Caffeine and alcohol act like mild diuretics and can aggravate urgency/frequency. Mayo Clinic+1

7) Move More: Walking, Strength, and Pelvic Floor Basics
- Walk daily (10–20 minutes) for weight, blood pressure, and mood. Mayo Clinic
- Light strength (2–3 days/week) supports insulin sensitivity and healthy body weight.
- Pelvic floor exercises (Kegels for men) can improve urgency/frequency and post-void dribble; coached training is helpful if symptoms persist. American University Alumni Network+1

8) Supplements: What’s promising—and what probably isn’t
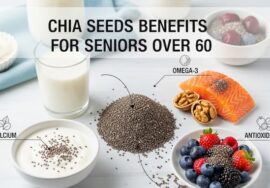
- Green tea catechins: interesting, but think “tea habit,” not high-dose capsules without clinician input. PMC
- Saw palmetto: large, high-quality trials show no better than placebo for BPH symptoms, even at higher doses—don’t delay care by relying on it. NCCIH
- Bottom line: “Food first,” and review any supplement with your clinician, especially if you take blood thinners or have chronic conditions.

9) Ben Stiller’s PSA Story (Hollywood reminder to get informed)
Actor Ben Stiller went public about his PSA test leading to an early prostate cancer diagnosis and successful treatment; his point wasn’t “everyone must screen,” but “know the discussion and make an informed choice.” In your 60s, that talk with a clinician is the move. Medium+1
10) A One-Week “Natural Prostate Routine” Starter Plan
Morning: 12–16 oz water → walk 10–20 min → oatmeal with berries & walnuts.
Midday: Big salad + beans/olive oil; green tea.
Afternoon: Strength mini-set (sit-to-stands, wall push-ups); practice 5 gentle pelvic floor squeezes. American University Alumni Network
Evening: Tomato-based entrée (chili, pasta sauce) with whole grains/veg; taper fluids 2–3 hrs before bed. PMC
Weekly: Weigh-in, medication review, and jot sleep/caffeine notes to spot patterns.

11) FAQs
Q1. What’s one simple daily habit for prostate comfort?
Hydrate earlier, taper fluids in the evening, and keep caffeine/alcohol modest and earlier in the day. Mayo Clinic
Q2. Are tomatoes actually helpful?
Food-based lycopene (tomato sauce/paste) is consistently linked with benefits; supplements are less clear. PMC+1
Q3. Should every man in his 60s get a PSA test?
Not automatically. The 55–69 group should decide with a clinician after weighing pros and cons. USPSTF+1
Q4. What’s a prostate-friendly coffee routine?
Smaller cups, earlier in the day, and try half-caf or decaf; avoid large late-night drinks. Mayo Clinic
Q5. Does saw palmetto work?
High-quality studies show no meaningful benefit vs placebo for urinary symptoms. NCCIH
Q6. Are green tea catechins worth it?
As a beverage habit, reasonable; high-dose supplements should be clinician-guided. PMC
Q7. Do pelvic floor exercises help men?
They can reduce urgency and leakage—especially with guidance. American University Alumni Network+1
Q8. Is a Mediterranean-style pattern useful?
Yes—more plants, olive oil, legumes, and fish supports vascular health and weight, which helps urinary comfort. Mayo Clinic
Q9. What’s a cheap “prostate-kind” dinner idea?
Tomato-bean chili with brown rice and frozen spinach—budget-friendly, fiber-rich. PMC
Q10. When should I see a urologist?
If you notice weak stream, straining, blood in urine, pain, fever, or weight loss—or if symptoms are disrupting life—book an appointment promptly. (Use the PSA discussion to decide about screening.) CDC
Trusted Outbound Resources
- Mayo Clinic – Enlarged prostate & diet tips (fluids/caffeine/alcohol, vegetables, exercise). Mayo Clinic
- USPSTF – Prostate cancer screening (55–69: individualized decision). USPSTF+1
- CDC – PSA screening talk with your doctor (updated 2025). CDC
- American Urological Association – Lifestyle measures for LUTS/BPH. American University Alumni Network
- NCCIH – Saw palmetto evidence summary (no better than placebo). NCCIH
- Peer-reviewed lycopene and green tea research. PMC+1
Internal reads (inbound links) to keepfitquote.com:




It’s laborious to search out knowledgeable individuals on this matter, but you sound like you recognize what you’re talking about! Thanks