Getting older changes how your pancreas works. This quiet, leaf-shaped organ sits behind your stomach and does two big jobs: it makes insulin to control blood sugar and digestive enzymes to break down fat, protein, and carbs. After 60—especially if you’re living with prediabetes or diabetes—insulin resistance tends to rise, enzyme output can slip, medications pile up, and small problems are easier to miss. The result? Subtle warning signs that many people chalk up to “just aging.”
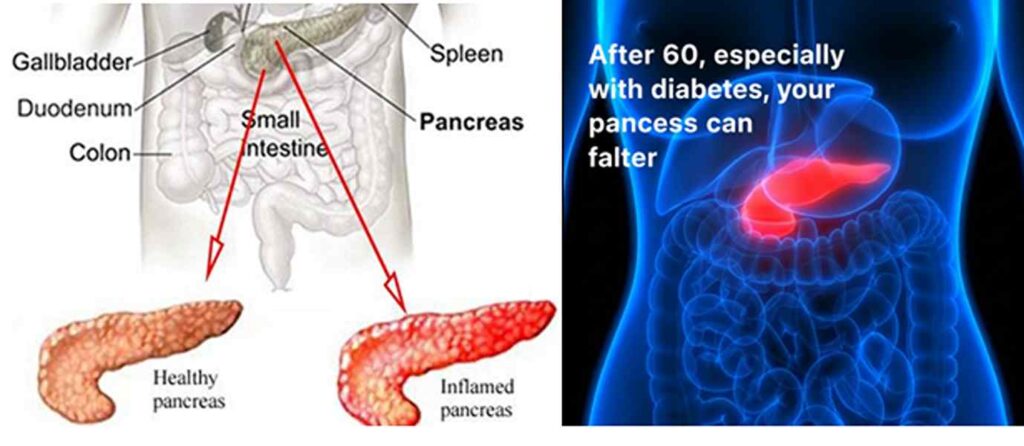
Table of Contents
- Quick Take
- Pancreas 101 after 60 (simple science)
- Natural warning signs in seniors
- When to call your doctor—red flags
- Lifestyle fixes: gentle, senior-friendly
- Food pattern for seniors & diabetics (sample day)
- Supplements & enzymes—what to ask your clinician
- Celebrity note (Hollywood): Tom Hanks & blood sugar awareness
- FAQs (10+)
1) Quick Take
- What matters after 60: Your pancreas helps digest food and regulate blood sugar. With age and diabetes, you may see digestive discomfort, unintended weight loss, greasy stools, or blood-sugar swings.

- Gentle fixes: Hydrate, walk daily, prioritize protein and fiber, choose heart-healthy fats, and space meds properly. If symptoms persist, seek medical evaluation.
- Diabetes nuance: Food timing, carb quality, protein at each meal, and consistent movement help reduce glucose spikes.

- Urgent signs: Persistent/severe upper-abdominal pain, fever, vomiting, jaundice, or dehydration—call your clinician or urgent care.

2) Pancreas 101 after 60 (simple science)
- Two jobs: (1) Digestive enzymes break down fat, protein, and carbs; (2) Hormones—especially insulin—help manage blood sugar.
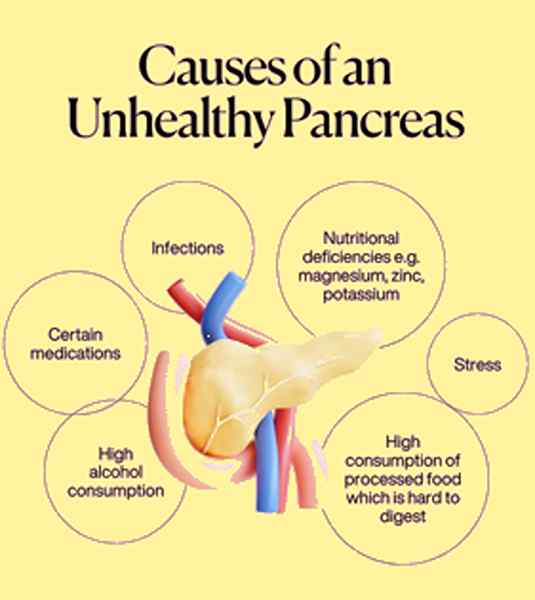
- Why seniors should care: Aging, medications, alcohol, gallstones, smoking history, or long-standing diabetes can stress the pancreas and affect digestion and glucose patterns.
Authoritative primers: NIDDK: Pancreatitis overview, NIDDK: Exocrine pancreatic insufficiency.
3) Natural warning signs in seniors
- Greasy, hard-to-flush stools (steatorrhea)—especially after fatty meals
- Bloating, gas, upper-abdominal discomfort that lingers after eating
- Unintended weight loss with normal eating
- Frequent diarrhea or pale stools
- Blood-sugar swings (more highs/lows than usual) despite similar meals
- Poor appetite or early fullness
If these persist for >2–3 weeks, schedule an evaluation. Learn more: Cleveland Clinic: EPI.

4) When to call your doctor—red flags
- Severe or persistent upper-abdominal pain (may radiate to the back)
- Fever, vomiting, dehydration, or fast heart rate
- Yellowing of eyes/skin (jaundice)
- Black or tarry stools, or blood in stool
- Sudden, significant unintentional weight loss
Reference: Mayo Clinic—Pancreatitis symptoms.

5) Lifestyle fixes: gentle, senior-friendly
- Hydrate on a schedule: Small, steady sips with meals and meds.
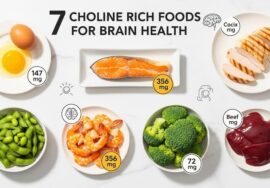
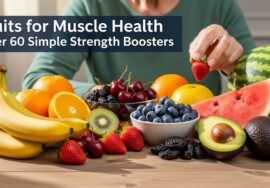
- Protein at each meal: Eggs, Greek yogurt, cottage cheese, tofu, fish, skinless poultry, lentils—easier glycemic control and better satiety.
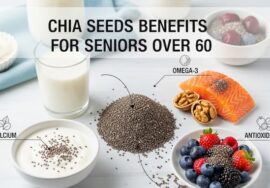
- Fiber without overload: Oatmeal, berries, apples, chia/flax (soaked), cooked veggies, beans in modest amounts—go slow to reduce gas.
- Fat quality + portion: Favor olive oil, avocado, nuts, baked/poached fish; limit deep-fried and heavy sauces if stools are oily/loose.
- Carb quality & timing: Choose low-GI carbs (oats, legumes, whole-grain toast) and pair with protein/fat to reduce spikes.
- Move after meals: 10–15 minutes of easy walking helps digestion and post-meal glucose.
- Alcohol & smoking: If applicable, reduce or avoid—both can worsen pancreatic stress.
- Medication spacing: Ask your clinician about timing with meals (especially diabetes, BP, GERD meds) to minimize symptoms and swings.
Helpful guidance: CDC—Diabetes management basics, ADA—Healthy eating & meal planning.
6) Food pattern for seniors & diabetics (sample day)
- Breakfast (soft & steady):
Warm oats + Greek yogurt + blueberries + 1 Tbsp soaked chia; cinnamon. - Lunch (digestive-friendly):
Baked salmon (or tofu) + quinoa + steamed zucchini + olive-oil drizzle. - Snack:
Cottage cheese + peach slices (or a small apple) + sprinkle of ground flax. - Dinner (light):
Poached chicken + mashed sweet potato + sautéed spinach (garlic, olive oil). - Evening walk: 10–15 minutes after dinner.

7) Supplements & enzymes—what to ask your clinician
- Prescription pancreatic enzymes may be suggested for EPI (exocrine pancreatic insufficiency)—only under medical supervision.
- Vitamin D & calcium: discuss lab checks and targets if bone health is a concern.
- B12 with metformin: long-term metformin can lower B12 in some—ask about testing.
Good starting points: NIDDK—EPI, AGA—Patient info on EPI.
8) Celebrity note (Hollywood): Tom Hanks & blood sugar awareness
Actor Tom Hanks publicly shared he has Type 2 diabetes and discussed weight changes over the years. His story highlights a practical lesson for seniors: steady weight management, routine labs, and consistent daily habits are more powerful than quick fixes. Coverage example: BBC News report.
9) FAQs (10+)
Q1. What are early pancreas warning signs in seniors?
Greasy stools, persistent bloating, upper-abdominal discomfort, unintended weight loss, or blood-sugar swings. If lasting >2–3 weeks, see your clinician.
Q2. What’s a gentle first step to “fix” symptoms naturally?
Simplify meals: protein + fiber + healthy fat, smaller portions, and short walks after meals. Hydrate steadily.
Q3. Can oily stools be a pancreas issue?
Yes—steatorrhea may indicate poor fat digestion. Ask about EPI and whether pancreatic enzymes are appropriate.
Q4. What breakfast is pancreas-friendly for diabetics?
Warm oats + Greek yogurt + berries + soaked chia. It’s soft, protein-rich, and steady on glucose.
Q5. How much fiber is too much for bloating?
Increase fiber slowly (a few grams/week) and soak seeds (chia/flax). Always pair with fluids.
Q6. Which fats are easier on digestion?
Olive oil, avocado, nuts, baked/poached fish—avoid heavy creams and deep-fried foods if stools are oily.
Q7. Does walking after meals really help blood sugar?
Yes—10–15 minutes can lower post-meal spikes and aid digestion.
Q8. Should seniors avoid all carbs for pancreas health?
No—choose lower-GI carbs (oats, legumes, whole-grain toast) and pair with protein/fat for smoother glucose.
Q9. When are enzymes considered?
If your clinician suspects EPI or you have malabsorption signs (weight loss, oily stools, deficiencies), prescription enzymes may help.
Q10. Are supplements necessary?
Only if deficiencies or clinical indications exist (e.g., Vitamin D, B12). Test first; supplement second.
Q11. Is alcohol a concern?
Alcohol can stress the pancreas; discuss reduction or avoidance with your clinician.
Q12. Any quick “pancreas reset”?
There’s no magic reset. Consistent gentle meals, hydration, daily movement, sleep, and medical follow-up work best.




I’m still learning from you, but I’m improving myself. I certainly enjoy reading everything that is written on your blog.Keep the posts coming. I liked it!